The picture most people paint when imagining a birth scene is one of a sweaty, screaming, red-faced woman lying on a hospital bed, the head of the bed elevated so she is upright just enough to look past her stirrup-supported legs at the doctor waiting to catch her baby. You know, just like our ancestors.
And though much of that scene comes from the images we are fed through movies and television, the part where the woman is on her back and her feet are in stirrups is, for the most part, accurate.
What position do most people give birth in?
In the 2009 Canadian Maternity Experience Survey, nearly all those who had a vaginal birth reported some variation of the above scene:1
- 9% reported lying flat on their back
- 8% reported being propped up on their backs or sitting
- Just 3.3% were side-lying, and 3.0% were in other positions
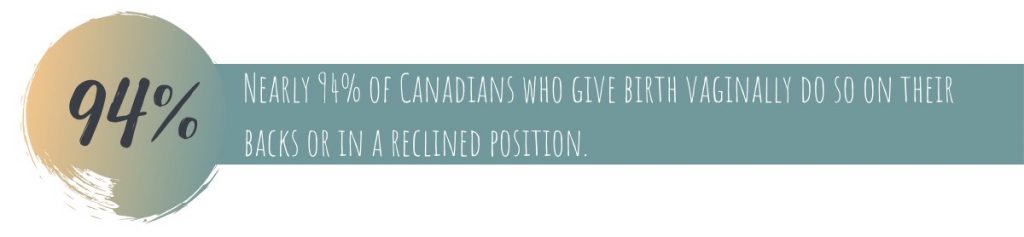
In the US, the major 2014 survey Listening to Mothers III reported a similar trend:2
- 68% reported lying flat on their backs
- 23% were semi-sitting (i.e. with the head of the hospital bed inclined)
- Just 3% were side-lying, 4% were squatting, and 1% were on their hands and knees
Why do most people birth while on their backs?
There are a few things at play:
- It is more convenient for the care provider during baby’s birth
- It is the position care providers are almost exclusively trained in and are therefore most comfortable with
- It is easier for caregivers to check baby’s heart rate throughout labour
- Caregivers may perceive that the use of epidurals and coinciding decreased mobility means that other positions aren’t possible
- Healthcare staffing limitations – those with epidurals may need extra assistance to be in more upright positions

Is there a better way?
The thing is, a lot of research has been done looking at those who are upright and moving during labour and there are benefits.
In an upright position (sitting on birthing stool/cushion, kneeling, hands-and-knees, squatting):3
- Gravity can help bring baby down and out
- There is less risk of compressing the pregnant person’s aorta, which means more oxygen for baby
- The uterus can contract more strongly and efficiently
- Baby can get in a better position
- The pelvic outlet can become wider (when squatting, kneeling, or on hands and knees)
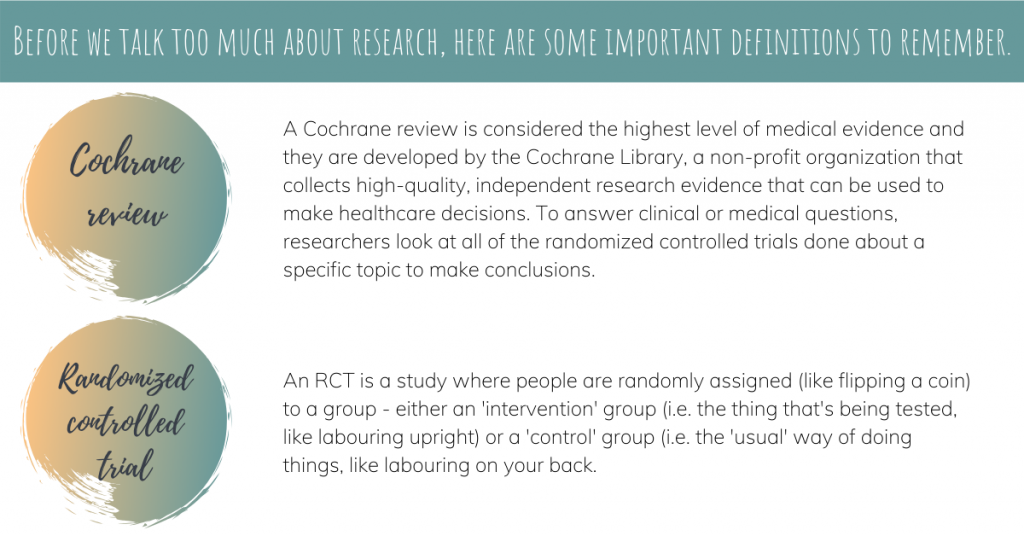
What do we know about upright movement while labouring?
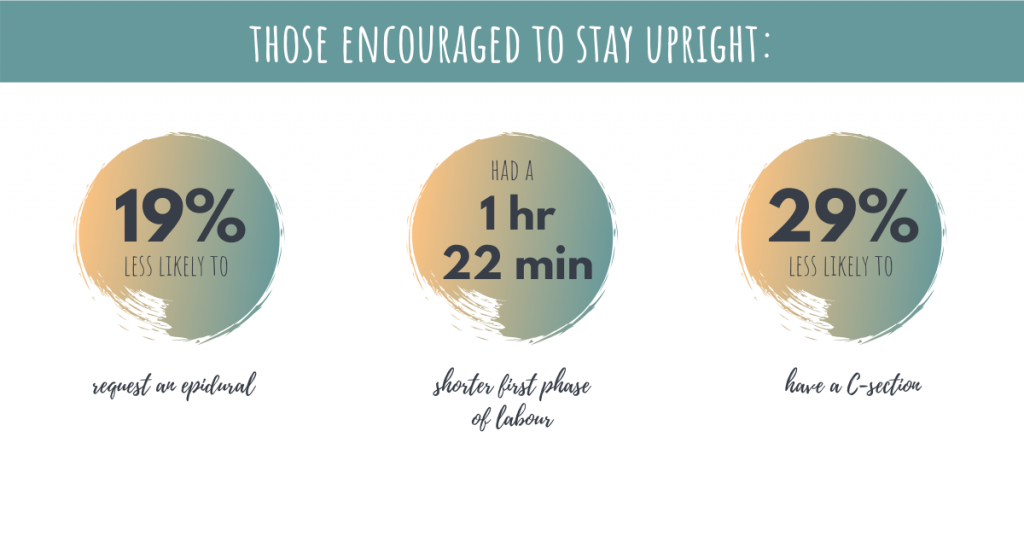
A 2013 Cochrane review (21 RCTs, 5218 people) looked at upright movement during the first phase of labour (0 – 10 cm dilation), before pushing.4
In these studies, people were randomly assigned to 1 of 2 groups. They were either encouraged to assume upright positions (walking, sitting, standing, kneeling) or to lie down (flat on their back, semi-reclined, on their side).
What do we know about upright positions once full dilation is reached?
The below studies focus on the second phase of labour, which starts once 10 cm of dilation is reached and ends when the baby is born. It includes the passive phase, where baby descends, followed by the active or ‘pushing’ phase.
Without epidurals:
A 2017 Cochrane review (32 RCTs, 9015 people) looked at studies where the birthing person was assigned an upright position for the second phase of labour (may or may not have birthed upright) vs. non-upright position.3
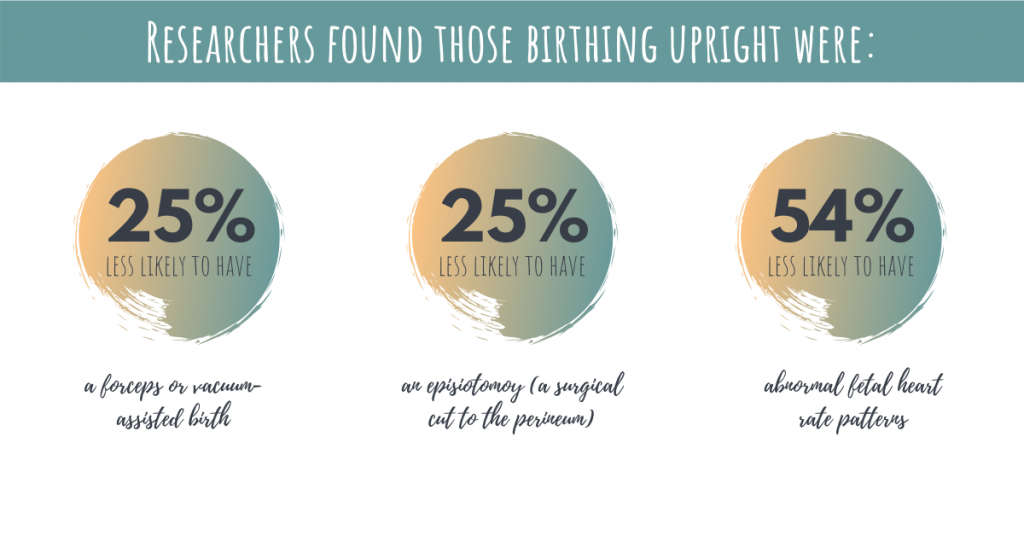
They were also:
- 20% more likely to have a 2nd-degree tear (15.3% vs. 12.7%, this is offset by the other group having more episiotomies – and research has found strong evidence that natural tears heal easier than episiotomies)
- 48% more likely to have estimated blood loss of more than 500 mL (6.5% vs. 4.4%, based on care provider estimates, which is not accurate. There was no difference in need for blood transfusions between groups)
With epidurals:
There is less conclusive research looking at this question for people who have epidurals.
A 2017 Cochrane review (5 RCTs, 879 people) compared people randomly assigned to upright versus not upright during the second phase of labour (but not necessarily during active pushing or birth) concluded that there was insufficient data to determine the effect of position for the second phase of labour in people with epidurals.5

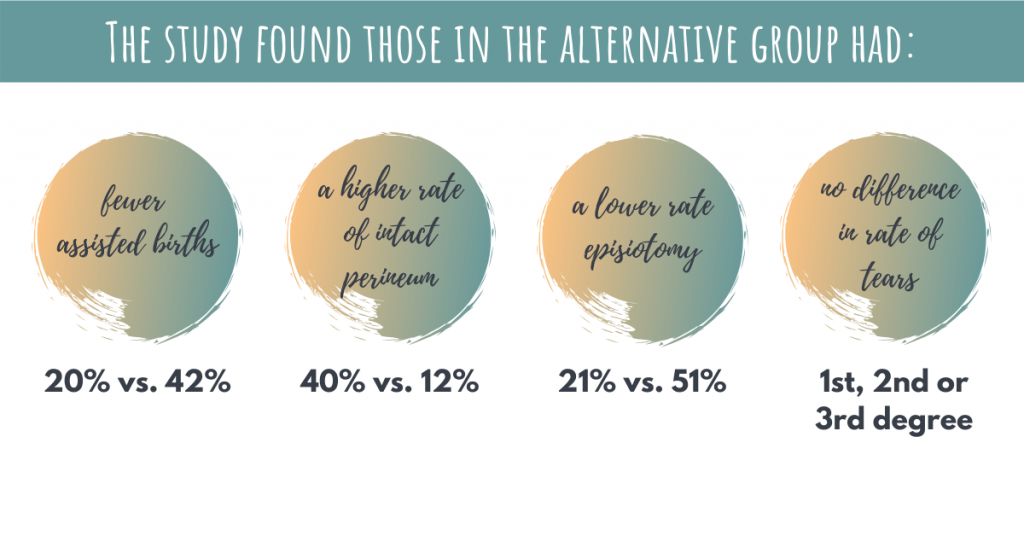
A 2012 study (199 people) assigned participants to 2 groups:6
- Traditional:
- Begin pushing (on back, head inclined, feet in stirrups) as soon as 10 cm of dilation is reached
- Give birth in this position
- Alternative:
- Begin pushing only after feeling a strong urge to push
- Change position every 20-30 minutes after full dilation is reached (sitting, kneeling, side-lying, hands and knees)
- If there is still no urge to push after 2 hours, start pushing with each contraction
- Give birth in a specific side-lying position (lower leg extended on bed, upper leg resting flexed, with foot higher than knee, in stirrup)
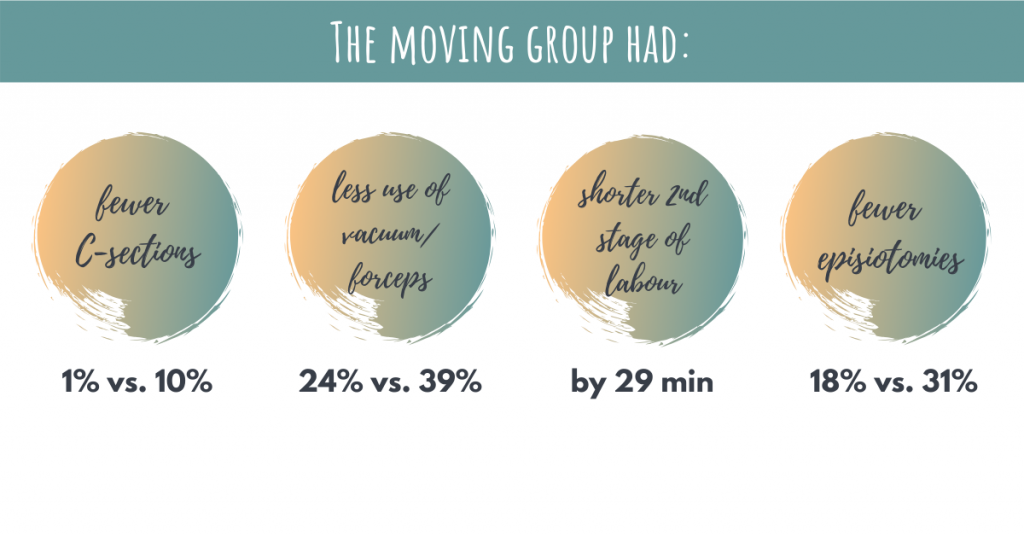
A second similar study from 2017 suggests these benefits can be achieved using only delayed pushing and position changes in the passive phase.7
In this study all participants delayed pushing and gave birth in the back-lying position described above, but one group made position changes and the other group didn’t.
What do the professional bodies say about positioning?
The Society of Obstetricians and Gynaecologists of Canada (SOGC) doesn’t have a formal recommendation on birthing position, but the Public Health Agency of Canada (2018) states that “Ideally, hospitals and birthing centres have equipment that enables women to give birth in different positions. Providers need to develop the necessary skills and knowledge to comfortably assist women to give birth in different positions and encourage women to be upright as this is optimal for birth”8
The Canadian Association of Midwives encourages free movement and instinctual behaviour in labour as well as spontaneous second stage pushing in the woman’s preferred position.9
In the US, the American College of Obstetricians and Gynecologists (ACOG, 2017) recommends that for most people “no one position needs to be mandated nor prescribed”10 and the WHO (1996) concludes that birthing people should adopt any position they like, preferable avoiding long periods of lying supine.11
What does all this information mean?
- There is no clinical recommendation stating that you have to lie on your back for your labour and delivery, nor is there evidence that it is safer for to do so. So listen to your body and do what is comfortable for you
- The benefits of movement and an upright birth can include shorter labours, less episiotomies, less instrumental birth, less C-sections, less pain, and more satisfaction
- Be mindful of interventions that require you to stay in bed (for example, ask for intermittent fetal monitoring or that it be wireless if continuous monitoring is indicated)
- Look for prenatal education classes that teach about movement and position changes in labour
- Consider hiring a doula – they are trained and knowledgeable about positions that are great for labour and can help nurture a supportive environment
- Some healthcare professionals are more flexible than others when it comes to birthing positions – midwives may be more accommodating than obstetricians in some cases
References: 1. Public Health Agency of Canada. What mothers say: The Canadian maternity experience survey. Ottawa (ON): 2009; 2. Declercq ER, et al. J Perinat Educ. 2014; 23(1):9-16; 3. Gupta JK, et al. Cochrane Database Syst Rev. 2017; 5:CD002006; 4. Lawrence A, et al. Cochrane Database Syst Rev. 2013; 8:CD003934; 5. Kibuka M, et al. Cochrane Database Syst Rev. 2017; 2:CD008070; 6. Walker C, et al. Int Urogynecol J. 2012; 23(9): 1249-1256; 7. Simarro M, et al. Med Sci (Basel). 2017; 5(1):5; 8. Public Health Agency of Canada. Family-centred maternity and newborn care: National Guidelines – Chapter 4. Ottawa (ON): PHAC: 2018; 9. CAM/ACSF Position Statement: Midwifery Care and normal birth. 2010; 10. American College of Obstetricians and Gynecologists. Am J Obstet Gynecol. 2019; 133:e164-173; 11. Technical Working Group, World Health Organization. Birth. 1997; 24(2): 121-123
Disclaimer: The information in this post absolutely does not constitute advice from a healthcare professional and is solely intended to provide you with general information. Each person is unique with individual circumstances, and as such some or all information may not apply to you.
This information does not substitute for your healthcare provider’s medical advice and should not be relied upon as such. Before making any decisions, be sure to reach out to a qualified healthcare professional. If you are pregnant and need to be examined, please see a physician, nurse practitioner, midwife or obstetrician.
We strive to ensure that the information provided is accurate, evidence-based, and reliable, but cannot guarantee that it is error-free or complete.